The Clinical Trials Support Office (CTSO) is the central hub for the trans-departmental Clinical Trials Support Units (CTSUs), providing enterprise-wide leadership, standards, policies, and a common infrastructure.

In our role as concierge for clinical research, we act as a liaison between Principal Investigators and study teams to other partners across the U-M involved in clinical research. At Michigan Medicine, all NIH-defined clinical trials and clinical research that has a billing calendar are required to be supported by a CTSU.
If you are a faculty or study team member, CLICK HERE to start the clinical research process, or connect with us at [email protected].

View the Michigan Medicine Clinical Research Site Profile for an overview of the resources we offer to support clinical research.
Our goal is easier and more timely navigation through the clinical research administrative process at Michigan Medicine.
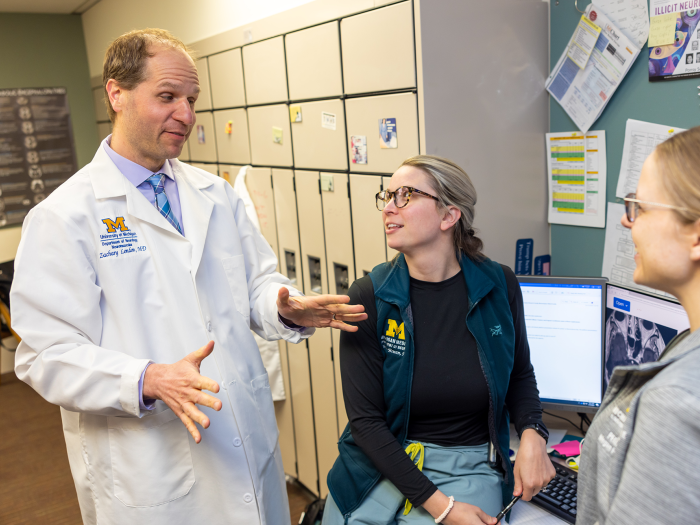
Clinical Trials Support Units (CTSUs) are business units that partner with investigators and their teams to ensure the timely and efficient activation and execution of clinical trials at Michigan Medicine.
Principal Investigators can ultimately find a smoother process and save time by taking advantage of our study coordinator pool, which can provide investigators with team members who are already on staff and fully trained.

The Michigan Clinical Research Unit (MCRU) provides clinical staff, resources, and infrastructure that are necessary to conduct adult and pediatric human clinical research protocols at the University of Michigan.

The Clinical Trials Support Office provides a structured and formalized path for developing faculty and study teams early in their career or new to clinical trial research.
The Clinical Trials Support Office and CTSU team members are here to help faculty and study teams easily and efficiently navigate the clinical research process, with greater support and increased satisfaction.
With this strong institutional backing of clinical research, Michigan Medicine is able to retain and recruit top-tier clinical scientists, improve our national visibility, and demonstrate the value of clinical trials to patients, families, and society.

O-CTSU: North Campus Research Complex, Building 300
2800 Plymouth Road
Ann Arbor, MI 48109
The Clinical Trials Support Office is a unit of the Medical School Office of Research, where our mission is to foster an environment of innovation and efficiency that serves the Michigan Medicine research community and supports biomedical science from insight to impact.







